Are you an avid runner? Have you been experiencing what may feel like calf pain at the beginning of, and after your workout?
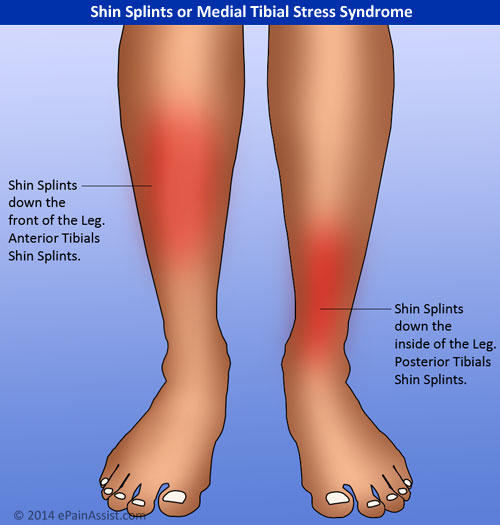
Something I have been treating a lot lately particularly in runners is a condition called Posterior Shin Splints aka Posterior Tibial Tendonitis or Posterior Tibial syndrome.
A Bit About Anatomy
The Tibialis posterior muscle lies deep to your tibia (shin bone.) It originates from the tibia and fibula above and is encased in an interosseous membrane. It attaches inferiorly to your foot, namely the navicular and medial cuneiform bones on the inside of the foot. The muscle serves to largely stabilize the lower leg and is also a very important stabilizer of the medial arch of the foot ( making it susceptible to injury in runners). It allows you to point your foot down and in (plantar flexion and inversion). Dysfunction of this muscle can lead to “flat feet.”
What’s Causing the Discomfort?
Injury to the muscle is typically an over-use injury. Many people will develop this problem when running with worn shoes, or when increasing mileage, or intensity via hill running etc. The problem ultimately develops from imbalances in other muscles in the lower leg. One of the culprits could be tight calf’s. The pain is typically felt on the medial side of the leg and may feel like calf pain that often travels down the inside of the leg. The pain occurs from inflammation of these tendons and increased friction. This can resemble stress fracture’s, so it is important to rule this out first!
What Can You Do to Fix It?
Stretch and re-educate the surrounding muscles namely the calf’s, tibialis anterior, peroneal, and foot muscles. Often Times, I will recommend the patient backs off of their mileage and seek other avenues to maintain their fitness such as swimming, or anything low-impact. Ice may be used in the initial stages if swelling is noted. Once swelling has reduced heat should be used to bring blood into the area and promote healing. Ultimately adhesions will develop due to inflammation of this area which will need to be addressed prior to regaining full mobility. For this, seek professional help from a licensed physician. I utilize myofascial release to break up adhesions prior to advising therapeutic exercise.
As always, please do not attempt to diagnose or treat any condition yourself without seeing a licensed professional.
Until Next Time!